National Pain Week
25-30 July
Exploring the 'Let them know how strong you are' theme.
Chronic Pain Australia wants to draw attention to the experience of people living with chronic pain and, by doing so, reduce the social and other barriers related to living and managing chronic pain.
This year’s theme ‘Let them know how strong you are’ and ‘painchanger’ aims to break down the stigma of talking about and seeking care for people experiencing chronic pain.
Many are taught to hide their pain for fear of appearing weak. The “she’ll be right” attitude is often adopted by Australians when addressing their chronic pain, leading to worsened, long-term impacts for both themselves, their family, friends, and colleagues. - Chronic Pain Australia
What is chronic pain?
Chronic pain is pain that lasts beyond normal healing time after injury or illness—generally
3 to 6 months.
In 2020, according to Australian Institue of Health and Welfare, 3.6 million Australians were living with chronic pain.
1 in 5 aged 45 and over are living with persistent, ongoing pain.
Of that, 53.8% are women -Pain Australia.
The Impact of Chronic Pain: Physical, Emotional, and Economic Aspects
How does chronic pain affect Australians?
Physical impact
Having chronic pain can reduce mobility and limit daily activities.
Sleep disturbances
Having constant pain makes it difficult to have restful sleep, as pain interferes with sleep, causing more pain, decreased energy and more fatigue.
Affects cognitive function.
Chronic pain makes concentrating, thinking or reasoning a challenge.
Chronic pain affects social activities.
Being physically active during family or social activities while suffering from chronic pain makes it almost impossible.
Emotional and psychological effects.
Having constant chronic pain can often lead to mood swings or emotions like anger and frustration, anxiety, stress, feelings of helplessness, depression and decreased quality of life.
Social isolation
People with chronic pain avoid social engagements and isolate themselves because of their condition. This leads to feeling isolated.
Substance misuse
Some individuals become dependent on the opioids prescribed to pain, while others self-medicate with alcohol or other drugs.
Economic burden
Australians with chronic pain face increased medical expenses.
“The total financial cost of chronic pain in Australia in 2018 was estimated to be $73.2 billion, comprising $12.2 billion in health system costs, $48.3 billion in productivity losses, and $12.7 billion in other financial costs, such as informal care, aids and modifications and deadweight losses.”
What is pain.
The International Association for the Study of Pain describes pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”.
How does pain work?
I’ve often compared pain to a black cloud over my head. Nobody else can see it, just me. But have you ever wonder what pain really is?
One of the best explanations I've heard about pain in a simple and easy way to understand is by Anjelo Ratnachandra who 'unpacks the changes that occur when pain changes from acute to chronic and provides an answer to common questions, such as why the weather or mood impact your pain experience'.
According to Pain Australia, there are 4 types of pain:
‘Acute pain
Pain that lasts for a short time and occurs following surgery or trauma or other condition. It acts as a warning to the body to seek help.
Sub-acute pain
Pain that is progressing towards chronic pain, but this progression may be prevented. This is known as the transition phase.
Recurrent pain
Pain that occurs on a cyclical basis, such as migraine or pelvic pain.
Chronic pain
Pain that lasts beyond the time expected for healing following surgery or trauma or other condition. It is often associated with an increased pain experience, not just in the area of injury, but also in surrounding tissue or nerves. It can also exist without a clear reason at all.’
Chronic Pain Types: Nociceptive, Neuropathic, Nociplastic
Chronic Pain Australia classifies chronic pain into 3 types:
Nociceptive
Neuropathic
Nociplastic
Nociceptive pain
“Nociceptive pain can be thought of as pain associated with tissue injury or damage or even potential damage. Nociceptors are sensory endings on nerves that can be excited or sensitised and signal potential tissue damage. Examples of different types of chronic nociceptive pain include osteoarthritis, pelvic pain, rheumatoid arthritis, and ankylosing spondylitis.
Neuropathic pain
Pain associated with injury or disease of nerve tissue. People often get this type of pain when they have shingles, sciatica, neck or back radiculopathy, trigeminal neuralgia, or diabetic neuropathy.
2. Neuropathic pain
Pain associated with injury or disease of nerve tissue. People often get this type of pain when they have shingles, sciatica, neck or back radiculopathy, trigeminal neuralgia, or diabetic neuropathy.
3. Nociplastic pain
Nociplastic pain is defined as ‘pain that arises from altered nociception despite no clear evidence of actual or threatened tissue damage causing the activation of peripheral nociceptors or evidence for disease or lesion of the somatosensory system causing the pain’.
This type of pain may reflect changes in the way the nervous and immune systems function. Examples of different types of chronic nociplastic pain include Complex Regional Pain Syndrome (CRPS), Fibromyalgia, and non-specific lower back pain.”
The Readiness Tool: Managing Daily 'Energy Budget' for Chronic Pain
One of the other videos I watched last year made a lot of sense. I had never thought about but do love and will try it out.
I’m talking about ‘The Readiness Tool.’
Here Brent Week, from Beyond Pain, talks about knowing your daily ‘energy budget’, i.e. how much energy you have to use in one given day. Using the Readiness Tool to establish a baseline, he recommends doing a test over a 3-month period. Brent compares 3 areas of energy to a traffic light system, you can watch the video belong which gives a clear explanation about this. Using this tool will give a clear understanding of “what you can do, not what your symptoms are doing.”
An example of a morning Readiness Tool, ticking off sleep quality, emotional heath and stress level.
If you would like a copy of this tool, please reach out by completing the from below.
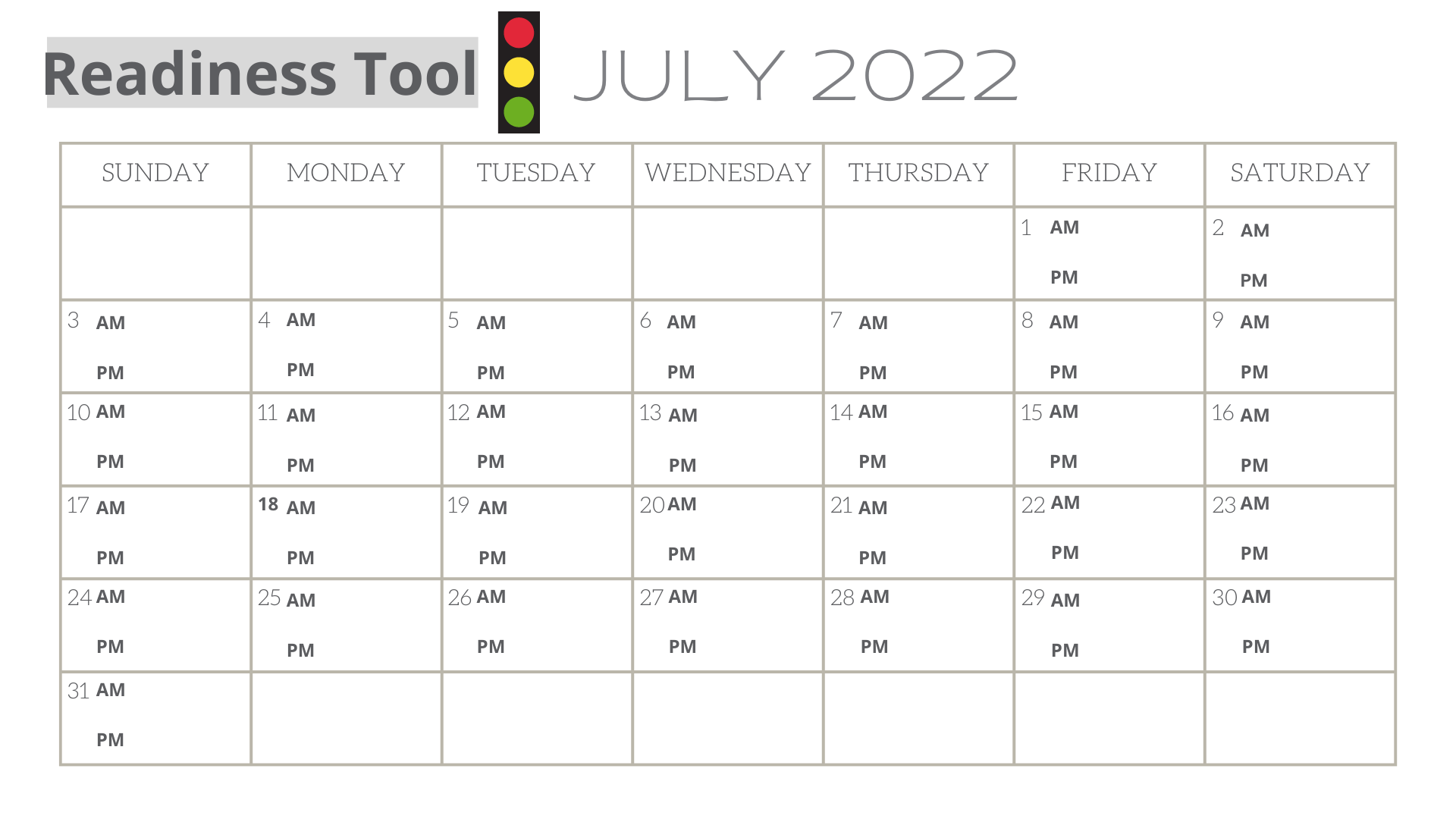
Start by using a calendar: digital or paper, and 3 coloured pens or highlighters: red, amber and green.
Start your day by tracking how you feel: green, amber or red, marking your intent for the day.
I also recommend marking how you slept, your emotional health, and stress level and mark those each out on your calendar. Using this info, you will then easily be able to note your exertion in a day, using the traffic light system again.
A flare-up is often an accumulation of multiple factors leading up to that flare-up, this will help give a clear indication, after 3 months, what causes your flareup.
An example of an evening Readiness Tool, marking off daily activity, expectations, if they were met and active rest, if taken.
If you would like a copy of this tool, please reach out by completing the form below.
An example of a daily Readiness Tool calendar marking off sleep quality, emotional health and stress level in the morning and then, in the evening marking off your daily activity, expectations, if they were met and active rest if taken.
If you would like a copy of this tool, please reach out by completing the form below.
Then at the end of the day mark your calendar with your green, amber or red on how the activity of your day went compared to the expectation of your day.
Did you overdo it or underestimate your energy?
The aim is to see a pattern: if your green days are always ending in red, then you are overdoing it.
The same can be said with starting with a red day. Do you have enough rest and recovery included on that day?
When you are ready to progress, do so at every level, green, amber and red.
Progression is very individual. Focussing on one factor only and increasing it between 10-20 % over 1-3 weeks. Obviously if you are starting your day and ending your day on red, you are not ready to progress and you really should listen to your body and try again a week later.
On your red days, Brent mentions having active rest days i.e. “meditation, body scanning, mindfulness, sleep or rest.”
Pain Management
Chronic Pain Australia recommends the following for ‘Good pain Management’:
Developing personalised and realistic goals
Developing a pain management plan that includes team-based care arrangements
Improving your knowledge and understanding of chronic pain
Supporting your skills and application of self-managing chronic pain
Reviewing and modifying your pain management plan
To find out what self-managing techniques Pain Australia suggests, click here.
Personal Experiences: Living with and Managing Chronic Pain
These are some ways I have found to relieve my pain. Please note this is from my personal experience and is not based on any medical science.
Pain is very individual. How one person reacts to pain is very different for another. Though I’m not a professional to supply you with medical knowledge of how to treat pain, I can only share my personal experience with pain and how I not only react to pain, but I usually do to relieve it.
Pain Relief Techniques: From Physical to Lifestyle Changes
Physical techniques
Get some sunshine
Getting outdoors
Laughter
Let’s face it, laughter makes everything better. Find people and things in your life that bring you joy and make you laugh out loud.
Walking
I have found that if I am bedridden, my pain increases. Please note, that there is a definite time and place when you do need rest, but long periods of bed rest are not the answer to reducing or relieving chronic pain.
Exercising
I do Pilates as my choice of exercise, as it includes strength, flexibility, and balance and it is definitely very gentle on my body.
Stretching
Great to do first thing in the morning, the last thing at night and during the day, whenever I need it.
If are you in need of seated neck stretches, click here.
Here are some neck stretches you can do whilst lie in bed.
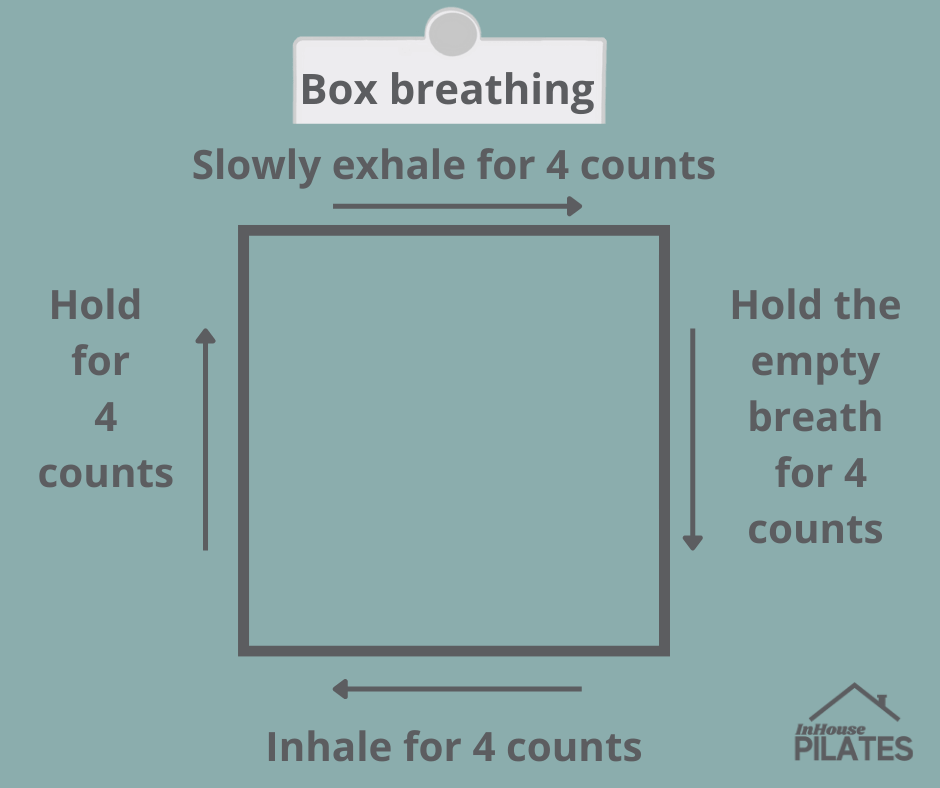
Deep breathing
Box breathing helps to bring my focus to my breath and not my pain.
Inhale for 4 counts,
Hold your breath for 4 counts,
Exhale for 4 counts,
Hold your empty breath for 4 counts. Repeat.
This breath has also helped me calm down when I am nervous or anxious.
7. Using hot or cold therapy.
As a general rule, you would use
a hot therapy like a warm shower which will help ease morning stiffness or use a heated wheat bag, or electric heating pads on the affected area.
cold therapy for joint pain, swelling and inflammation. Use either a bag of frozen veggies or a gel ice pack wrapped in a tea towel. The idea is only to cool the area for at least 15 minutes not freeze the area. NEVER apply ice directly onto the skin as you will end up with an ice burn.
8. Acupuncture or dry needling
9. Remedial massage
10. Bowen therapy
11. Cognitive behaviour therapy
Lifestyle changes
12. Eat an anti-inflammatory diet
13. Sleep
One of the major factors that increase my pain levels is poor sleep.
Factors that improve good sleep are:
is banning electronics in the bedroom, and maintaining a regular sleep schedule for going to bed and getting up.
I sleep with an eye patch to block out any light and use earplugs to block out any noise.
14. Reduce stress
This is a biggie! Apart from sleep, reducing stress is a must to relieve chronic pain. If not the chronic pain circle continues.
15. Magnesium
16. Fish oils
I recently read an article written by Dora Chan, Pharmacist, Functional Medicine Nutritionist about how to reduce pain naturally, you can read about it here.
As part of using the Readiness Tool, Brent Week has recommended to use, I also recommend using a Pain diary.
Nothing is worse than being in pain and not being able to see a doctor immediately. By the time that you do see a doctor, you’ve forgotten the what, the where and the why of your pain.
Pain diary: A comprehensive approach to tracking pain details
For this very reason, I have created a Pain Diary. One single place where you can make notes about your pain details and have them ready to take with you on your next doctor’s visit.
If you would like a copy of the Pain Diary in pdf form, and how to use it, just complete the form below and I am happy to send you a link where you can print this off as many times as you need it.
In conclusion, please find help dealing with your pain, either via your doctor to refer you to a Pain management team to help and support you.
If you need further support, please contact the relevant link below to get the right help that you deserve.
SUPPORT SERVICES
Chronic Pain Australia cannot offer clinical advice to individuals or their families living with chronic pain. We can, however, connect you to updated information or services that can support or assist you in managing your pain experience better. Depending on your circumstances, you may find the following information helpful.